Wearable Device for the Early Detection of Common Diabetes-related Neurological Condition
About Optica
28 July 2014
Wearable Device for the Early Detection of Common Diabetes-related Neurological Condition
FOR IMMEDIATE RELEASE
Contact:
Lyndsay Meyer
The Optical Society
+1.202.416.1435
lmeyer@osa.org
Wearable Device for the Early Detection of Common Diabetes-related Neurological Condition
Hooked onto glasses, new optical device may be able to detect diabetic autonomic neuropathy sooner, leading to better treatment outcomes
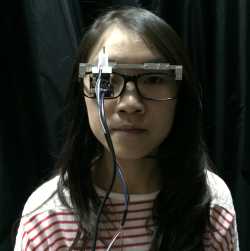
A prototype pupillometer designed for a patient to wear for a half hour or so in a doctor's office and test for diabetic autonomic neuropathy. It may help diagnose the condition sooner, leading to better treatment outcomes. Credit: M. Ou-Yang, National Chiao-Tung University, Taiwan.
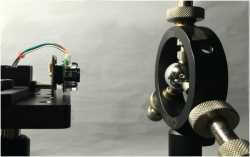 The original experimental set-up of the pupillometer, which has since been prototyped for patient wear (see image 1). On the right is an eye model, and on the left is the pupillometer device, including its infrared LEDs and CCD camera. Credit: Applied Optics.
The original experimental set-up of the pupillometer, which has since been prototyped for patient wear (see image 1). On the right is an eye model, and on the left is the pupillometer device, including its infrared LEDs and CCD camera. Credit: Applied Optics.Described in a paper published today in The Optical Society (OSA)’s journal Applied Optics, the new technology is a small, wearable device called a pupillometer that can hang on a pair of eyeglasses and only weighs 78 grams, slightly heavier than Google Glass. Developed by a team at National Taiwan University Hospital, Hsin Chu branch and National Chiao-Tung University, the device is designed to be worn for a half hour or so in the doctor's office, during which time it would monitor a person's pupils. By carefully measuring five parameters associated with the pupils, doctors may then be able to detect the earliest signs of diabetic autonomic neuropathy.
Detecting someone's asymptomatic diabetic autonomic neuropathy early and treating it properly may lead to far better health outcomes for them. Currently the condition is often not detected until moderate nerve damage and organ dysfunction are present.
Currently doctors rely on observing changes in digestive speed, heart rate and blood pressure to detect diabetic autonomic neuropathy, but this limits their ability to make a diagnosis early on, said Mang Ou-Yang, who led the research with colleagues at National Chiao-Tung University. Now they have shown that monitoring the pupils of people with diabetes may be a better approach.
"Compared to the existing diagnostic techniques, the pupillometer is a more reliable, effective, portable and inexpensive solution for diagnosing diabetic autonomic neuropathy in its early stages," said Ou-Yang.
The pupil is useful for detecting diabetic autonomic neuropathy due to the neurological conditions caused by the disease. Like many organs, the eyes and pupil are dually innervated, receiving signals from both the parasympathetic and sympathetic divisions of the autonomic nervous system. These divisions control the pupil’s circular and radial muscles, respectively.
The pupillometer, which is small enough to be mounted onto the front of a pair of glasses, works by emitting four colored lights to stimulate the pupil. A beam splitter attached to the device then filters the visible light that is reflected from the eye to the device’s camera, which processes the images to analyze the pupil’s size.
The device measures 10 parameters related to pupil diameter and response time. Of those 10, the researchers found that five parameters were significantly different in people with diabetic autonomic neuropathy.
Ou-Yang says if clinical trials are successful, the pupillometer could be available by the end of the decade.
Future research for Ou-Yang and his lab includes scaling down the size of the device, expanding the device’s capabilities to observe two pupils simultaneously and collecting more experimental results from diabetic patients.
Paper: “Design and analysis of wearable pupillometer for autonomic neuropathy of diabetic patients,” M.-L. Ko et al., Applied Optics, Volume 53, Issue 29, pp. H27-H34 (2014).
EDITOR’S NOTE: Images are available to members of the media upon request. Contact Lyndsay Meyer, lmeyer@osa.org or 202.416.1435.
About Applied Optics
Applied Optics publishes articles emphasizing applications-centered research in optics, moving the potential of science and technology to the practical. Published three times each month, Applied Optics reports significant optics applications from optical testing and instrumentation to medical optics...from holography to optical neural networks...from LIDAR and remote sensing to laser materials processing. Each issue contains content from three divisions of editorial scope: Optical Technology; Information Processing; and Lasers, Photonics and Environmental Optics. It is edited by Joseph Mait of the U.S. Army Research Laboratory. For more information, visit www.OpticsInfoBase.org/AO.
Founded in 1916, The Optical Society (OSA) is the leading professional society for scientists, engineers, students and business leaders who fuel discoveries, shape real-world applications and accelerate achievements in the science of light. Through world-renowned publications, meetings and membership programs, OSA provides quality research, inspired interactions and dedicated resources for its extensive global network of professionals in optics and photonics. For more information, visit www.osa.org.
